Improve your billing speed & accuracy
ArogyaMD Medical billing software ensures that your patient billing process runs smoothly every time

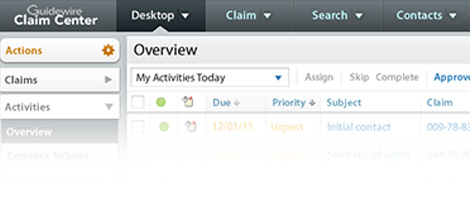
Manage your entire claim process in one place
ArogyaMD gives you all the tools you need to manage your claims process—in one place. Other medical billing systems force you to manually export and upload claims to separate or multiple clearinghouses. The Claims Center™ powerful automation manages all these tasks for you behind the scenes.

Auto-generates worklists
The system automatically builds actionable work lists that allow you to quickly identify and fix claim errors, exclusions or denials.

Tracks payment status
The system automatically tracks the status of payment, time, exclusions, payers and more.

Centralized billing
For billing professionals, Centralized Billing features allow you to manage claims processing for your clients.
Review, edit & approve charges online
The ArogyaMD allows for a quick final review of all charges that have been captured. Quickly make edits while in the review screen, saving valuable time. You can also set user preferences that allow charges to bypass review if needed.
Identify claim issues before submission
Claim Inspector™ automatically scrubs claims for potential errors. It runs more than 3.5 million edits on each claim for CCI, HIPAA, LCD and carrier-specific requirements before the claim is submitted. As a result, we GUARANTEE our customers’ first-pass claim acceptance rate is 95% or better.

Submit, review & edit
Within ArogyaMD.com you can also batch process Payments and Receipts directly through our integrated system. The system takes care of sending and receiving information between you and your payers. Plus, when it receives ERA information, it builds actionable work lists that make managing billing errors and rejections painless.
Automate your patient billing process
Process statements, send gentle reminders to collect money in an electronic format and write off specific accounts to a collection agency file—all from one screen. Additionally you can place an account on hold from receiving notifications and customize how many statements a patient receives before receiving a collection letter.

Patient statements
Review key information about each account, such as the account type, the date and amount of the last responsible party payment that was received, any unapplied money sitting in the account, and the balance owed on the statement.

Send soft collection letters
This do-it-yourself option gives you all the tools to automate and manage collection letters easily. You can create customized letters suited to each responsible party. No need to use a third-party agency.

Write off overdue accounts
Simply check a box to have a collection agency file created during your billing run. You can configure the billing rules to write off a portion or complete account balances. A downloadable file is generated that can be sent to your agency.

Batch process patient billing
Batch process or perform the billing run with the single mouse click. You can download the collections file, view summaries of billing runs and print paper statements all from this screen.

Process credit cards
Process credit cards stored on file. You can choose to charge responsible parties for the outstanding patient balance up to the maximum available amount. View patient balances and select which cards to charge.

Generate payment plan statements
You can generate payment plan statements separately from regular statements. Create default and custom payment plan groups, add messages to statements and preview statements before processing.